But yes, it's #BusinessAsUsual because #Crapitalism requires people to #ConsumeConsumeConsume!
Canadian teen with #BirdFlu was on #LifeSupport, new report reveals
The hospitalized teen was also given three #antiviral treatments, underscoring how severe #H5N1 infection can be
By Nicole Karlis, January 6, 2025
"In November, a teenager in British Columbia was infected and hospitalized with bird flu, caused by the H5N1 virus. While most cases have been mild, commonly characterized by #conjunctivitis and respiratory symptoms, this previously healthy Canadian teen was hospitalized from the virus in critical condition. Their symptoms started with double conjunctivitis, also known as pink eye, and turned into a fever and coughing. A few days later the teenager was admitted to intensive care after developing acute respiratory distress syndrome [#ARDS].
"'This was a healthy teenager prior to this, so no underlying conditions,' said British Columbia’s health officer, Bonnie Henry, at a news conference at the time. 'It just reminds us that in young people this is a virus that can progress and cause quite severe illness.'
"Now, a recent report brings to light more details about the teenager’s case. In the report, published in the New England Journal of Medicine (NEJM), researchers explain that the 13-year-old girl spent weeks fighting for her life after contracting a severe H5N1 infection from an unknown source. In finding her diagnosis, researchers say that she initially tested positive for influenza A, but not the seasonal subtype. Further testing suggested she had a high viral load of a novel influenza A infection, which researchers discovered to be the H5N1 avian flu.
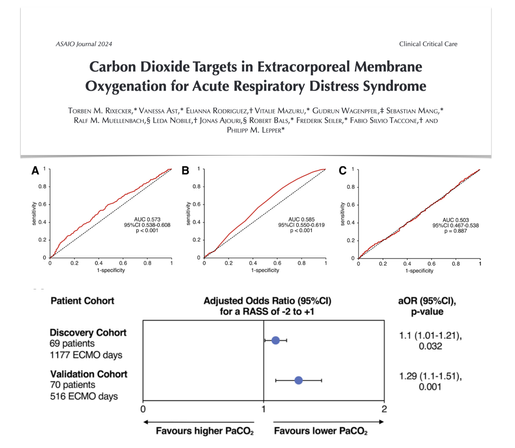
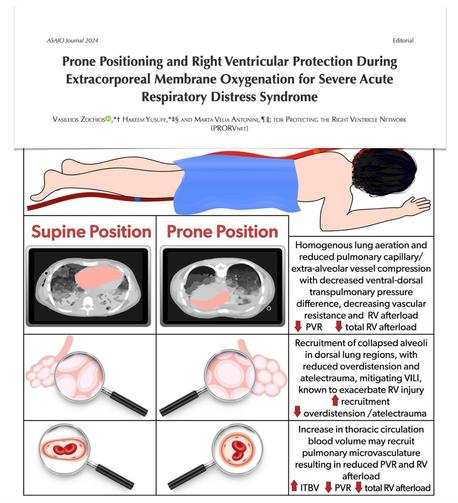
"The next day doctors started her on oseltamivir, also known under the brand name Tamiflu. However, her respiratory functions declined rapidly causing her to be intubated. She was also placed on extracorporeal membrane oxygenation (ECMO), a machine that is a form of life support for people with life-threatening illnesses. In addition to the ECMO machine, the teenager received a plasma exchange and two more antiviral medication treatments — amantadine and baloxavir.
"In an accompanying editorial, experts noted while mutations were detected in her case, it’s 'unclear whether these #mutations were present in the infecting virus or emerged during the course of the patient’s illness.'
"In other words, it’s unclear if the virus #mutated to be more severe in humans.
"'The mutations evident in the Canadian case highlight the urgent need for vigilant surveillance of emerging mutations and assessment of the threat of human-to-human transmission,' the editorial stated, adding that vaccine development and therapeutics are also needed — perhaps to treat more severe illness. 'The Canadian case showed higher viral loads in the lower airway and very prolonged shedding, despite therapy, which highlights the potential need for longer therapy.'
"Researchers concluded their editorial with an acknowledgment that 'many questions remain.' For example, the severity of cases is likely to depend on host immunity, the route of exposure, or other changes in the virus.
"Currently, the CDC says that the risk to most Americans remains low.
"'We do have candidate vaccines and antivirals available to try to mitigate severe influenza in the case of wider spread,' the report stated. 'That said, a balance between enhanced vigilance and ‘business as usual’ is needed."
https://www.salon.com/2025/01/06/new-report-on-severe-case-of-canadian-teen-with-bird-flu/
#HPAI #BirdFluMutations #Flu