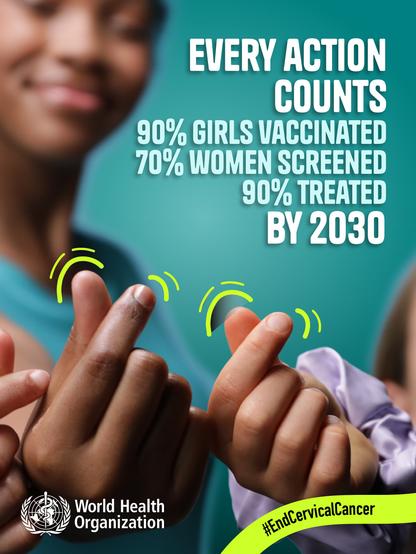
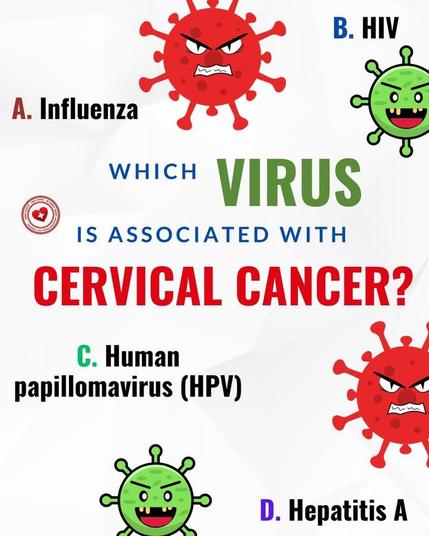
💡 Cervical cancer screening just got easier. New ACS guidelines now allow self‑collection for HPV testing, expanding access and reducing barriers. Clear stopping rules at age 65 help avoid unnecessary tests.
Read more ➡️ https://blog.banishcancer.org/cervical-cancer-screening-guidelines-accessibility-updates/
#CervicalCancer #HPVTesting #CancerPrevention #HealthcareAccess #ScreeningGuidelines #BanishCancer