#healthSystems
How much does climate change really cost our health?
In many African regions, the answer is already becoming clear: rising temperatures, shrinking water sources, food insecurity, and the spread of diseases like malaria are putting intense pressure on health systems. These aren’t separate problems—they’re all deeply connected.
In our new article (with Walter Leal, Gouvidé Jean GBAGUIDI, Wassa Diarrassouba), we explored how climate change is driving up health costs across Africa. Using spatio-temporal mapping and a broad review of the literature, we show how these impacts are growing over time and space—and why it’s urgent to act now.
https://pimmartens.com/2025/03/27/how-much-does-climate-change-really-cost-our-health/
#GlobalHealth #ClimateJustice #PlanetaryHealth #Africa #ClimateChange #HealthSystems #Malaria #OneHealth
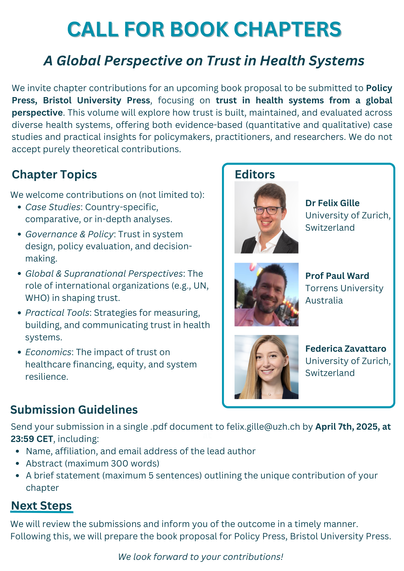
📢 Call for Chapter Abstracts – Trust in Health Systems
Seeking abstracts for A Global Perspective on Trust in Health Systems, a proposed edited volume with Policy Press. The book will explore how trust is built, maintained & evaluated across diverse health systems.
📅 Deadline: April 7, 2025
Africa: A Wake-Up Call for Resilient Health Systems in Africa: [allAfrica] Last month, the United States, the largest global health donor, accounting for 32% of all international health assistance, announced its withdrawal from the World Health Organization and issued a blanket stop-work order at USAID, threatening critical health programs. http://newsfeed.facilit8.network/THmPx7 #AfricaHealth #GlobalHealth #HealthSystems #USAID #WHO
Africa: Bolstering Health Systems With Genomic Surveillance - Insights From the Genmoz Project: [Malaria Consortium] How training health workers and leveraging data-driven insights are reshaping malaria control efforts in high-burden regions of Mozambique. http://newsfeed.facilit8.network/THcntX #Africa #HealthSystems #GenomicSurveillance #MalariaControl #DataDriven
Africa: Africa Must Take Full Charge of Its Health Systems: [New Times] The recent decree by newly sworn-in US president, Donald Trump withdrawing the United States from the World Health Organisation (WHO), while unfortunate, presents a unique opportunity for Africa to strengthen its own healthcare systems and prioritise continental self-reliance. http://newsfeed.facilit8.network/THX6Th #AfricaHealth #SelfReliance #PublicHealth #HealthSystems #WHO
The following hashtags are trending across South African Mastodon instances:
#dreamed
#epidemicpreparedness
#publichealth
#healthsecurity
#globalhealth
#onehealth
#COVID19
#healthsystems
#womeninhealth
#internationalcooperation
Based on recent posts made by non-automated accounts. Posts with more boosts, favourites, and replies are weighted higher.
🌍 International Day of Epidemic Preparedness: December 27, 2024 🌍
Today, we emphasize the critical importance of investing in robust health systems to prevent, detect, and respond to infectious disease outbreaks. The ongoing COVID-19 pandemic has shown us the devastating effects of epidemics on lives and economies. It’s essential to build resilience in our public health systems to safeguard communities, especially the most vulnerable.
🔍 Key Points:
Global health crises disrupt lives and economies, highlighting the urgent need for effective epidemic management.
Collaboration at all levels—local, national, and international—is vital for successful responses.
An integrated One Health approach is necessary, considering the interconnectedness of human, animal, and environmental health.
Gender perspectives must be incorporated in epidemic management, recognizing the crucial role of women in healthcare.
The UN, particularly the WHO, plays a pivotal role in coordinating global responses to epidemics.
Let’s unite in awareness and action to strengthen our preparedness for future health threats.
Join us in observing this important day!
#EpidemicPreparedness #PublicHealth #HealthSecurity #GlobalHealth #OneHealth #COVID19 #HealthSystems #WomenInHealth #InternationalCooperation #UNGA #SCABPharmacy
Why guidelines fail: on consequences of the false dichotomy between global and local knowledge in health systems
Global health continues to grapple with a persistent tension between standardized, evidence-based interventions developed by international experts and the contextual, experiential local knowledge held by local health workers. This dichotomy – between global expertise and local knowledge – has become increasingly problematic as health systems face unprecedented complexity in addressing challenges from climate change to emerging diseases.
The limitations of current approaches
The dominant approach privileges global technical expertise, viewing local knowledge primarily through the lens of “implementation barriers” to be overcome. This framework assumes that if only local practitioners would correctly apply global guidance, health outcomes would improve.
This assumption falls short in several critical ways:
- It fails to recognize that local health workers often possess sophisticated understanding of how interventions need to be adapted to work in their contexts.
- It overlooks the way that local knowledge, built through direct experience with communities, often anticipates problems that global guidance has yet to address.
- It perpetuates power dynamics that systematically devalue knowledge generated outside academic and global health institutions.
The hidden costs of privileging global expertise
When we examine actual practice, we find that privileging global over local knowledge can actively harm health system performance:
- It creates a “capability trap” where local health workers become dependent on external expertise rather than developing their own problem-solving capabilities.
- It leads to the implementation of standardized solutions that may not address the real needs of communities.
- It demoralizes community-based staff who see their expertise and experience consistently undervalued.
- It slows the spread of innovative local solutions that could benefit other contexts.
Evidence from practice
Recent experiences from the COVID-19 pandemic provide compelling evidence for the importance of local knowledge. While global guidance struggled to keep pace with evolving challenges, local health workers had to figure out how to keep health services going:
- Community health workers in rural areas adapted strategies.
- District health teams created new approaches to maintain essential services during lockdowns.
- Facility staff developed creative solutions to manage PPE shortages.
These innovations emerged not from global technical assistance, but from local practitioners applying their deep understanding of community needs and system constraints, and by exploring new ways to connect with each other and contribute to global knowledge.
Towards a new synthesis
Rather than choosing between global and local knowledge, we need a new synthesis that recognizes their complementary strengths. This requires three fundamental shifts:
1. Reframing local knowledge
- Moving from viewing local knowledge as merely contextual to seeing it as a source of innovation.
- Recognizing frontline health workers as knowledge creators, not just knowledge recipients.
- Valuing experiential learning alongside formal evidence.
2. Rethinking technical assistance
- Shifting from knowledge transfer to knowledge co-creation.
- Building platforms for peer learning and exchange.
- Supporting local problem-solving capabilities.
3. Restructuring power relations
- Creating mechanisms for local knowledge to inform global guidance.
- Developing new metrics that value local innovation.
- Investing in local knowledge documentation and sharing.
Practical implications
This new synthesis has important practical implications for how we approach health system strengthening:
Investment priorities
- Funding mechanisms need to support local knowledge creation and sharing
- Technical assistance should focus on building local problem-solving capabilities
- Technology investments should enable peer learning and knowledge exchange
Capacity building
- Training should emphasize critical thinking and adaptation skills as constitutive of new forms of leadership
- Learning programmes should connect peers across contexts
- Evaluation should measure local innovation and problem-solving
Knowledge management (KM)
- Systems need to recognize that knowledge is found in the connections between humans (and increasingly machines), so that improving KM is about more ‘pipes’ (connections) and better quality-ones
- Platforms should therefore enable peer learning and exchange
- Evidence must include practitioner experience and insights
New paths forward
Moving beyond the false dichotomy between global and local knowledge opens new possibilities for strengthening health systems. By recognizing and valuing both forms of knowledge, we can create more effective, resilient, and equitable health systems.
The challenges facing health systems are too complex for any single source of knowledge to address alone. Only by bringing together global expertise and local knowledge can we develop the solutions needed to improve health outcomes for all.
References
Braithwaite, J., Churruca, K., Long, J.C., Ellis, L.A., Herkes, J., 2018. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med 16, 63. https://doi.org/10.1186/s12916-018-1057-z
Farsalinos, K., Poulas, K., Kouretas, D., Vantarakis, A., Leotsinidis, M., Kouvelas, D., Docea, A.O., Kostoff, R., Gerotziafas, G.T., Antoniou, M.N., Polosa, R., Barbouni, A., Yiakoumaki, V., Giannouchos, T.V., Bagos, P.G., Lazopoulos, G., Izotov, B.N., Tutelyan, V.A., Aschner, M., Hartung, T., Wallace, H.M., Carvalho, F., Domingo, J.L., Tsatsakis, A., 2021. Improved strategies to counter the COVID-19 pandemic: Lockdowns vs. primary and community healthcare. Toxicology Reports 8, 1–9. https://doi.org/10.1016/j.toxrep.2020.12.001
Jerneck, A., Olsson, L., 2011. Breaking out of sustainability impasses: How to apply frame analysis, reframing and transition theory to global health challenges. Environmental Innovation and Societal Transitions 1, 255–271. https://doi.org/10.1016/j.eist.2011.10.005
Salve, S., Raven, J., Das, P., Srinivasan, S., Khaled, A., Hayee, M., Olisenekwu, G., Gooding, K., 2023. Community health workers and Covid-19: Cross-country evidence on their roles, experiences, challenges and adaptive strategies. PLOS Glob Public Health 3, e0001447. https://doi.org/10.1371/journal.pgph.0001447
Yamey, G., 2012. What are the barriers to scaling up health interventions in low and middle income countries? A qualitative study of academic leaders in implementation science. Global Health 8, 11. https://doi.org/10.1186/1744-8603-8-11
Share this:
#climateChangeAndHealth #decolonization #evidenceBasedInterventions #expertise #globalHealth #healthSystems #implementationScience #localKnowledge